Developing story
Mpox outbreak in DR Congo: What to know
A recent surge of mpox (formerly known as monkeypox) infections in DR Congo is cause for alarm. Here’s what to know and why we need a comprehensive response.

Developing story
A recent surge of mpox (formerly known as monkeypox) infections in DR Congo is cause for alarm. Here’s what to know and why we need a comprehensive response.
The mpox epidemic currently sweeping through Democratic Republic of Congo (DRC) is spreading at an alarming rate—and has been reported beyond DRC's borders.
Since the beginning of this year, there have been close to 20,000 cases of mpox and over 630 deaths, according to Congolese authorities. While epidemic outbreaks are generally concentrated in the center and northwest of the country, confirmed cases of mpox have now been reported in the eastern provinces of South and North Kivu, where almost a million displaced people are living in overcrowded conditions. The epidemic now affects all provinces in the country and, following a genetic mutation in South Kivu, has been causing uninterrupted human-to-human transmission of the virus for months.
patients treated in MSF-supported facilities since June
awareness sessions held, reaching over 1 million people
contact cases currently receiving in-home follow-up
Since June 17, Doctors Without Borders/Médecins Sans Frontières (MSF) has been mobilizing emergency teams to respond to the mpox epidemic across the country. Our teams are on the ground in South Kivu, North Kivu, Equateur, and South Ubangi provinces to support the local health authorities. More than 1,400 patients have been treated in MSF-supported facilities since June.
On August 14, the World Health Organization (WHO) director-general declared that the surge of mpox cases in DRC and a growing number of countries in Africa constitutes a public health emergency of international concern. The emergency declaration followed advice from an expert committee warning that the disease has the potential to spread further across countries in Africa and possibly outside the continent. On September 13, WHO announced that the MVA-BN vaccine is the first vaccine against mpox to be added to its prequalification list. The MVA-BN vaccine can be administered to people over 18 years old as a two-dose injection given 4 weeks apart.
As this disease continues to spread, here’s what to know about mpox in DRC.
Photo above: DR Congo 2024 © Michel Lunanga
Mpox is a disease caused by the monkeypox virus. It is transmitted by close contact between people or with infected animals. It has been endemic in Central Africa (strain I) and West Africa (strain II) since the 1970s, and spread rapidly around the world in 2022-2023, with tens of thousands of cases linked to the West African variant reported in more than 110 countries.
Common symptoms of mpox are rashes, lesions, and pain, which can be managed with supportive care to help ease symptoms and avoid complications. Vaccines to prevent the spread and therapeutics to treat people who fall ill are only available in some countries. Most patients recover within a month, but some infected people get very sick and even die. The current outbreak in eastern DRC is caused by a new offshoot of clade 1, called clade 1b, which causes more severe disease than clade 2. More than 479 people have died since the start of this year. In comparison, the WHO estimates that mpox claimed the lives of 89 people worldwide in 2022.
The main source of transmission is sexual, but it is also still being transmitted in the traditional ways: through direct or indirect contact with blood, body fluids, skin lesions, or mucous membranes of infected animals. Secondary or person-to-person transmission can occur through close contact with infected secretions from the respiratory tract or skin lesions of an infected person, or with objects recently contaminated by a patient's fluids or lesion material.
Although mpox is endemic (meaning a disease that exists permanently in a given area) in 11 of DRC’s 26 provinces, the number of cases has been rising sharply for over two years. Health authorities in DRC declared an epidemic in December 2022. The number of mpox cases tripled in 2023, with more than 14,000 suspected cases reported and 511 deaths. In 2024, the situation has worsened further: between January and the beginning of August, more than 14,000 suspected cases were reported across 23 provinces.
The extremely limited availability of mpox vaccines in DRC has already drastically reduced the reach of the national strategic plan for vaccination against mpox. Vaccines must arrive in the country as quickly as possible so we can protect people in the areas most affected, particularly the most at-risk populations such as Congolese health workers, who are on the front line of the infection, as well as sex workers and displaced people living in camps. DRC has validated two mpox vaccines and is trying to obtain supplies, but at this stage there are still no vaccines available for people in the country. Negotiations are underway with other countries and priority areas are being identified.
The acceleration of the epidemic amid a slow rollout of vaccines is worrying, especially due to a genetic mutation identified in South Kivu. Previously, outbreaks of mpox were mostly related to zoonotic transmission, from animals to humans. Now the disease has been transmitting from humans to humans in a sustained manner for months. In South Kivu, for example, the disease has been spreading across multiple health zones since last year, exclusively from person to person—through both sexual contact as well as close household contact.
Another cause for concern is that the disease has been recorded in camps for displaced people around Goma, capital of North Kivu province, where extreme population density and high rates of sexual violence make the situation critical. There is a real risk of an exploding number of cases given the significant population movements in and out of DRC. However, the identification of cases, the monitoring of patients, and the care available remain extremely limited in DRC. The lack of vaccines makes the situation even more difficult. In some communities, there is a perception that the disease is linked to mystical practices, which also complicates adherence to public health measures. Community trust is also a key part of an effective outbreak response.
MSF has responded to mpox outbreaks for years, including in DRC in 2022 and 2023, and the Central African Republic in 2018. We're stepping up our efforts in light of the way the mpox epidemic is developing.
The current mpox epidemic in DRC is spreading in areas with significant demographic and geographical differences, requiring a multifaceted response adapted to each context. We need as many partners as possible to support key aspects of controlling the epidemic, including laboratory analysis, surveillance, support for isolation and self-isolation, and awareness-raising in communities. All of these areas suffer shortcomings and require significant resources to function properly.
Since mid-June, one of our teams has been supporting Uvira health zone in South Kivu, and assisting the medical management of severe cases through an isolation center at the Uvira General Referral Hospital, as well as monitoring simple and moderate cases on an outpatient basis and isolating suspected cases. Our teams are training medical staff on medical management and are also involved in infection control and raising awareness in communities. We are also providing hospitals with kits for treatment and for taking samples of the disease. In Minova, our teams set up an isolation center at the general reference hospital.
In Goma, North Kivu, we have launched surveillance and awareness-raising activities in camps for displaced people where we are present. We are strengthening the capacity of health structures to manage triage, isolation, and the treatment of patients presenting symptoms of mpox.
In the northwest of DRC, two other interventions have been launched: one in the Bikoro health zone in Equateur and the other in the Budjala health zone in South-Ubangi. This time, operations will be long-term, lasting several months. We also aim to train medical staff in medical and psychological care and step up epidemiological surveillance and infection prevention and control, including community awareness-raising—particularly for people who are sometimes harder to reach, such as people with disabilities. In Budjala, more than 550 patients were treated with our support between mid-June and mid-July. In Equateur, we will be conducting operational research with the health authorities to better understand the dynamics of the virus and combat the disease.
Stopping transmission will require a comprehensive response, with communities at the center. MSF calls on all stakeholders to rapidly support all pillars of the mpox response—including health promotion and community engagement, surveillance, targeted vaccination, diagnostics, and treatment. The response must ensure the equitable distribution of resources to the communities most affected.
September 05 09:48 AM
Controlling the mpox outbreak will be impossible unless living conditions are improved.
Read More
August 16 09:10 AM
With the mpox outbreak in DR Congo continuing to evolve rapidly, access to vaccines is critical to curb further spread of the virus.
Read More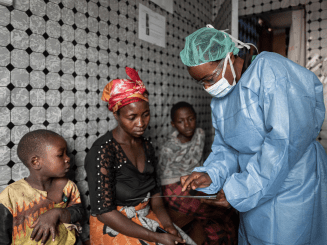
July 30 10:11 AM
An MSF medical coordinator explains the recent surge of mpox in DR Congo, where a new mutation has led to human-to-human transmission.
Read More