Nearly 20 percent of Rohingya refugees tested in the camps of Cox's Bazar, Bangladesh have an active hepatitis C infection, according to a recent study carried out by Doctors Without Borders/Médecins Sans Frontières (MSF) and Epicentre, the organization's epidemiology and medical research arm.
These refugees have been living in precarious conditions since 2017 after fleeing targeted violence and persecution in neighboring Myanmar. Now they are trapped in camps they cannot leave and reliant on humanitarian aid. But lifesaving screening, testing, and treatment services are nearly non-exisent in Cox's Bazar, and MSF is the only provider of hepatitis C care for thousands of people in the camps. In light of the alarming findings of the study, we are urgently calling for other actors to step up and help provide hepatitis C care.
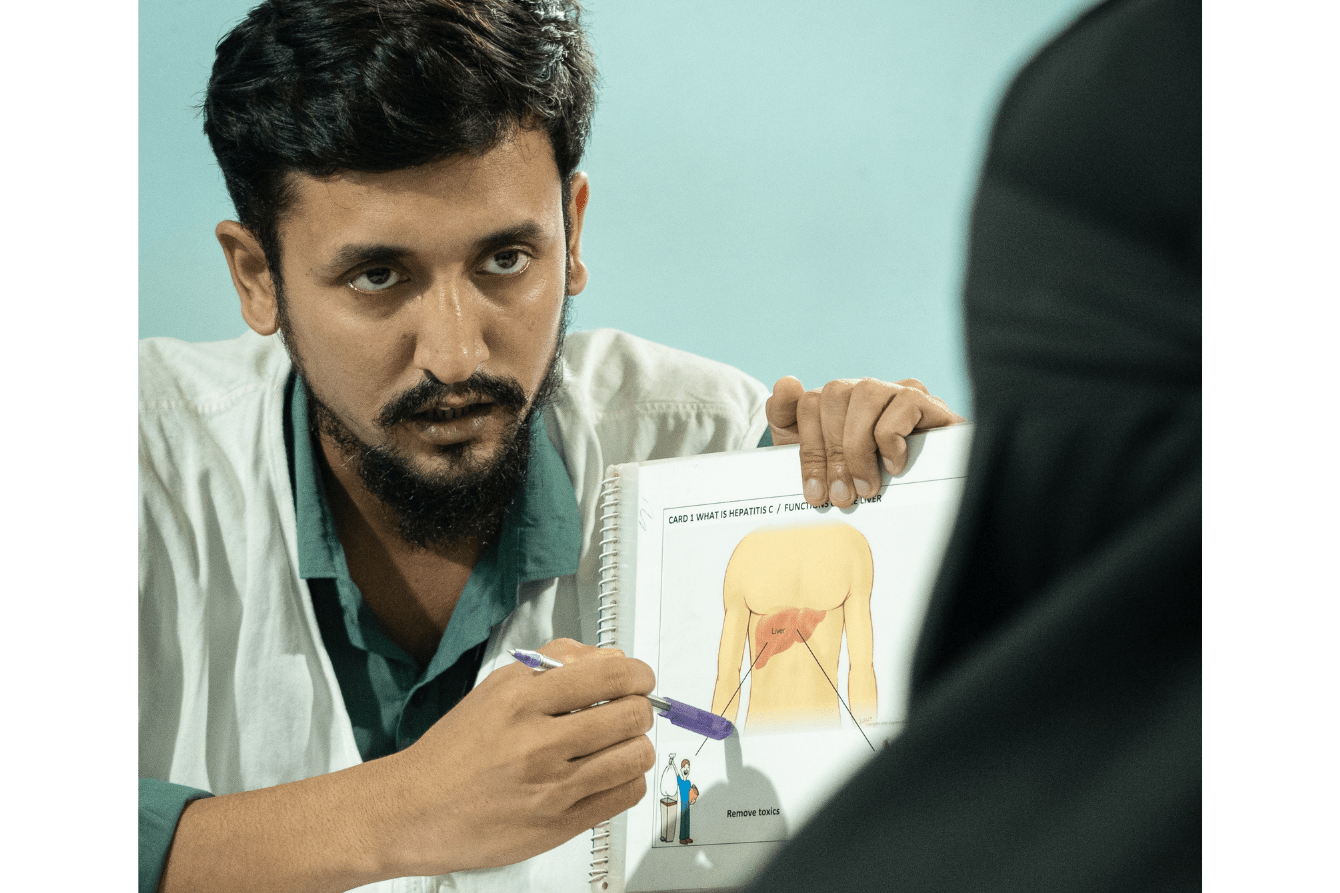
"Every day, hundreds of patients line up in a seemingly endless queue outside the MSF specialized clinic in Cox's Bazar in the hope of being cured," explained Dr. Wasim Firuz, deputy medical coordinator at MSF. "They have witnessed the devastation caused by hepatitis C, having lost family members here or when they were living in Myanmar."
For the past four years, Dr. Firuz and his team have been able to treat only a tiny proportion of the Rohingya refugees affected by this infectious disease, which is often diagnosed in several members of the same family. This is the case of Mujibullah, whose wife and two sisters are infected with the hepatitis C virus (HCV). His mother, who has now died from it, was worried that the virus would spread to the whole family, and about the cost of treatment.

A recent survey carried out by MSF and Epicentre in the camps of Cox's Bazar reveals that at least one in three Rohingya adults has been exposed to the virus and almost one in five has chronic active hepatitis C, amounting to an estimated 86,000 individuals. Since October 2020, MSF has seen more than 8,000 patients—between 150 and 200 new patients every month—but even this number of consultations is not sufficient to meet the needs.
"In the five or six months before I started HCV treatment, I felt so bad that I couldn't even get to the market right next door to us," said Shamsul, a father of five who has been living in the camp since 2017. "Every time I thought about the journey, I felt like I was going to collapse on the road; I was weak, tired, and nauseous. I took the treatment for three months and felt better. The tiredness, loss of appetite, and pain gradually disappeared."
Massive need for treatment in the camps
Hepatitis C is bloodborne and is usually transmitted through the use of unsterilized needles and unsafe medical practices. According to the study carried out by MSF and Epicentre, exposure to these practices could be the main risk factor in the specific and confined context of the camps.
Around 70 percent of the people who took part in the MSF study reported having received therapeutic injections, either in the camps in Bangladesh or in Myanmar, often in medical establishments, from traditional healers, or during childbirth carried out in the traditional way. Harsh living conditions in cramped and overcrowded camps, lack of access to health care, reduced provision of health care, and lack of legal status have made Rohingya refugees more vulnerable to infections, including hepatitis C.
"After experiencing the symptoms of hepatitis C, I consulted a traditional healer to obtain herbal remedies,” said Shamsul. “These remedies, made from vines and scales of plants, tasted very bitter. My wife, who also had hepatitis C, took them and felt better. Encouraged by her improvement, I started taking them. At first we felt some relief, but after a few days the symptoms returned, and my wife began to experience symptoms similar to mine."
"Hepatitis C has become a major concern for the whole community,” said Baduran, a community health worker with MSF. "Seeing people’s pain and frustration breaks my heart. As a member of this community, I share their struggles. I wish we could treat everyone, but we can't. The fear of hepatitis C remains, a constant reminder of the difficult choices we face."
Effective treatment, but limited access
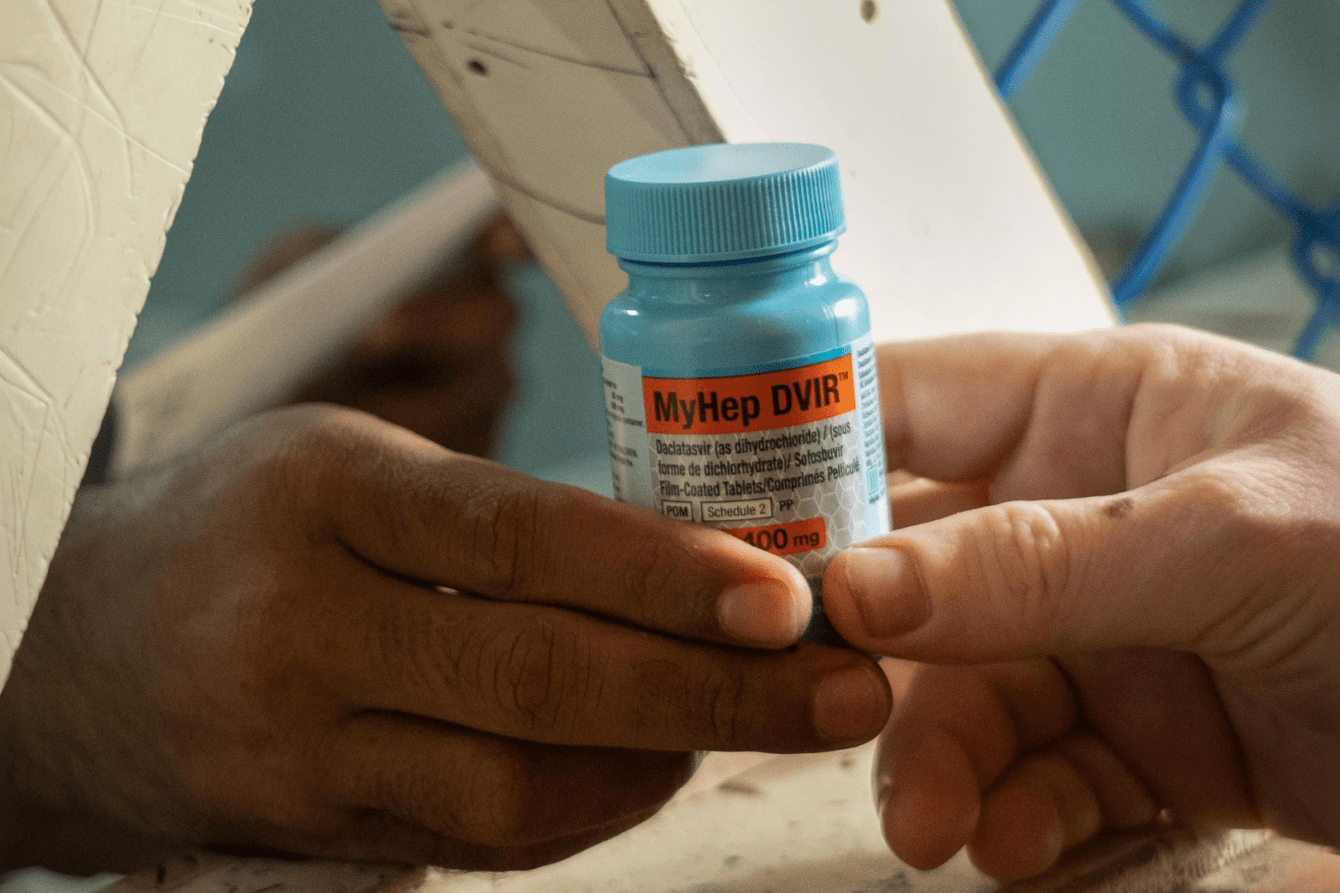
Access to diagnosis and treatment remains inadequate in many low- and middle-income countries, as is the case in Bangladesh. In 2022, the World Health Organization (WHO) estimated that hepatitis C had led to the deaths of 242,000 people worldwide, mainly from complications such as cirrhosis and liver cancer. Since 2014, direct-acting antivirals have made it possible to treat hepatitis C effectively. MSF teams used these treatments to treat around 19,000 people in Cambodia between 2016 and 2021. MSF decided to launch a simplified model for the treatment of hepatitis C in the Rohingya community of Cox’s Bazar in 2020, based on the one in Cambodia.
"This model is based on the use of rapid diagnostic tests and a reduced number of follow-up visits and tests," explained Dr. Farah Hossain, MSF medical programs deputy manager. "This means that treatment initiation is faster and extremely effective."
"From the outset, it was clear that demand for hepatitis C treatment was high in the camps, with very long queues," added Dr. Hossain. "There was an urgent need to understand the burden of the disease by estimating the number of people requiring diagnosis and treatment."
Although Bangladesh has a plan to combat viral hepatitis, the cost of diagnosis and treatment remains high. Each diagnostic test costs US $20 and each person tested must be tested twice, which means a total cost of $40 US per person, further increasing the already steep medical costs for patients.
"HCV treatment has only been available at the MSF hospital, which makes it difficult for people to access the medicines they need to be cured and have a chance of survival before it gets worse," said Shamsul.
"Unfortunately, we cannot treat everyone because of limited resources. We treat people aged between 40 and 70," said Dr. Wasim. "Younger people have a chance of self-remission and it usually take years for them to develop complications, while older people are more vulnerable."
Breaking the chain of transmission
Enormous progress has been made in the treatment of hepatitis C in recent years, with success rates of up to 95 percent thanks to the new direct-acting antivirals. This rate is also being observed by MSF teams in the camps of Cox's Bazar. A massive HCV testing and treatment campaign needs to be implemented in all Rohingya refugee camps in Bangladesh, which requires a rapid increase in access to testing and treatment.
"At the same time, we need to break the chain of transmission through a large-scale prevention and health promotion campaign," said Dr. Hossain. "A multi-partner initiative involving humanitarian and health players is needed to coordinate these efforts."
Most people with HCV have no symptoms until the disease becomes serious, threatening their lives after many years of progression, leading to jaundice or liver cancer.
"If HCV is detected and treated in time, it can be eliminated, thereby preserving the health of the liver," said Dr. Hossain. "In the long term, the integration of hepatitis C treatment in all health centers is necessary to prevent new cases and break the transmission chain."
MSF is currently working with the Bangladesh Ministry of Health to draw up a national plan for the treatment of hepatitis C based on the simplified treatment model implemented in the camps.

Rohingyatographer: Sharing the Rohingya story in photos
Read moreThe simplified model of care, ready to be shared with all the medical actors in the camps, should facilitate the use of HCV tests and treatment. Health education campaigns are needed to address the lack of information on HCV prevention in the camps. Community activities to combat stigma and discrimination must also be implemented.
"The announcement that WHO, Save The Children, and the International Organization for Migration are opening a program to combat hepatitis C in the Cox's Bazar camps is an important step in the right direction," said Dr. Hossain.
"Many people in our camp share this silent struggle," said Jafar, a Rohingya refugee cared for by MSF. "Tests confirm the presence of the virus, but treatment remains costly. One thing is certain: there is a cure and many people have recovered. That's the hope I'm clinging to. The hope that one day the medicine my wife desperately needs will be available."




